GETTING FIT ONE STEP AT A TIME
Walking, you do it every day. Just putting one foot in front of the other, however, can do more than get you from point A to point B. Done intentionally, walking can transform your obdy and lengthen your life. A brisk 20-minute walk could have significant health benefits. According to the National Institutes of Health, walking may:
- Lower your risk of health problems like high blood pressure, heart disease and diabetes.
- Strengthen your bones and muscles
- Help you burn more calories
- Lift your mood
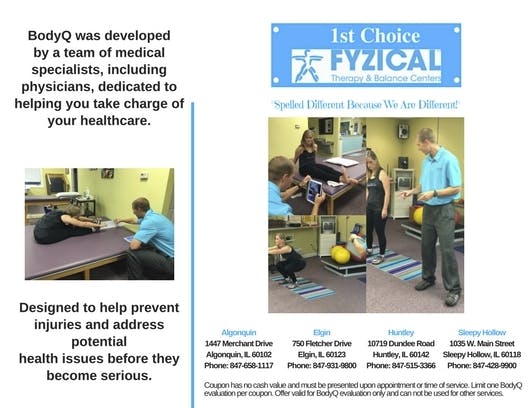
If you've been sedentary, consider having a gait analysis before you get started. This is especially important if you're in rehab or have any discomfort in walking. The Journal of Nutrition, Health and Aging has reported that gait velocity, or how fast you walk, correlates to fall risk," says Tina Schmidt MPT, Assistant General "Manager of Physical Palm Beach. "BODYQ by Physical measures gait velocity to see if you are at risk and also assess overall muscular imbalances to determine the best exercises to develop the strength, coordinate and balance to safely return to a walking program."
As an exercise, walking workouts are not meant to be an easy stroll through the park. You could, of course, walk anywhere: park, mall beach or street. That's what makes walking workouts so convenient. But it's how you do it that transforms walking into an effective fitness-building activity.
Walking workouts are brisk and intentional aerobic activities. Thus, your heart rate should rise to a moderate cardiovascular level. A simple way to know if you are in a moderate cardiovascular zone is if you can talk but not sin while walking. Singing requires more cardiovascular effort and more lung capacity. So, your breathing is clue: if you can smoothly sing a tune, you need to amp up your walk.
GET A SHOE THAT FITS
Just as gait analysis can help prevent an injury, the right shoes make all the difference. Trying shoes on at the end of the day is a good strategy because that is when you feet are at their largest. Look for shoes that allow you to wiggle your toes but not slide around inside. The shoes should also provide some cusHioning and light treads on the bottom to prevent slipping while walking. Running shoes could work, but be mindful that the larger treads can be a tripping hazard.
STAYING SAFE AND INJURY FREE
Proper walking form is important. Keep your chin up and your shoulders slightly back. Let the heel of your foot touch the ground first, and then roll your weight forward. Walk with your toes pointed forward and let your arms swing naturally.
Keep your feet happy by wearing sweat-absorbent socks and keeping your toe nails trim to avoid ingrown toenails. Stretching is vital for your whole body, including your feet. Stretching may help you avoid plantar fasciitis and tightness in the Achilles tendons and shin splints.
"A gentle stretch can help ease next day soreness," says Schmidt. "An easy leg stretch can be done while laying on your back and extending your leg up to the ceiling. Point and flex your foot to stretch out the front and back of the leg."
Avoid talking on a cellphone while workout walking. Just like talking and driving, chatting on the phone while workout walking is a major distraction. Focus on your body and your surroundings instead. It will help keep you safer and reduce your risk of stumbling off a curb or into an opening car or shop door.
If you're going to be walking in the early morning or later at night, a safety vest, which reflects the light of oncoming cars,m is an inexpensive accessory to wear. Dawn and dusk make it harder for drivers to see you, and while you're smart enough not to be distracted by chatting on a cell phone, the same is not sure of a lot of drivers. If you're going to walk near traffic or on the road, wear reflective clothing.
EASY WAY TO INCREASE INTENSITY
To increase your intensity, you can simply walk faster. But weights can be a great addition to a walking workout program. A pair of light hand weights can help increase your effort and help strengthen your arms, too. You don't need a lot of weight, a couple of 2 or 3 pound dumbbells are enough. Some are made with walking workouts in mind as they are easy to hold and have foam covers for a nonslip grip. Weighted vests are another option. These vests have slots where you can place the amount of weight you'd like. Weighted vests are quite practical because you can add weight as you walking workouts get easier. In addition, you make just about any workout more intense, for example, doing push-ups or riding your bike becomes more challenging wearing a weighted vest.
Walking sticks are also quite useful especially if you have slight balance issues or are trekking over uneven terrain. The sticks can also make it easier on your knees when you go up and down hills.
GADGETS GALORE TO TRACK YOUR STEPS AND MORE
To keep yourself motivated and on task, create some goals and chart your progress. Tracking your time, steps and distance area all ways to mark your accomplishments. There are many trackers out on the market. Among the most basic are pedometers, which just track your steps. It's a simple way to ensure you've done at a set amount of steps per day. A pedometer is an inexpensive tracker that can motivate you to go around the block just one more time to complete your daily goal.
On the other side of the scale, are more comprehensive devices that track time, steps, distance and heart rate, offer GPS routs and much more. Of course, they can also cost $150 and up. Many can automatically chart your data through online applications. They also typically offer online communities where you can make virtual friends to support and challenge you.
Finally, if you need motivation to get or keep moving, consider signing up for a fundraising walk. there are many charities that have walking events nationwide. What a great way to raise money for your favorite cause and provide you with a reason to keep on moving!